- This page was created by volunteers like you!
- Help us make it even better. To learn more about contributing to MEpedia, click here.
- Join the movement
- Visit #MEAction to find support or take action. Donate today to help us improve and expand this project.
- Congratulations!
- MEpedia has got over 30 million views as of August 2022!
John Chia
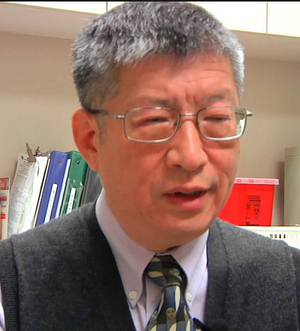
Dr. John K. S. Chia is an infectious disease doctor with a medical practice in Torrance, California. Dr. Chia became heavily involved in research and clinical care of myalgic encephalomyelitis (ME) and chronic fatigue syndrome (CFS) patients after his son, Andrew Chia, became ill with CFS in 1997. He has published several papers[1] on infectious causes of ME and CFS, including evidence of involvement of enteroviruses such as coxsackie B and echovirus, other viruses such as parvovirus B19, as well as bacteria such as Chlamydia pneumoniae. In addition to his clinical work, he runs his own enterovirus research laboratory[2] and is on the board of directors of the Enterovirus Foundation.
Dr. Chia has performed clinical trials[3] in an attempt to find treatment for patients with ME and CFS. His treatment attempts have focused on the use of antiviral compounds such as amantadine, ribavirin, and lamivudine in addition to immune modulators such as interferon and the plant compound oxymatrine. Towards this end, he and his son, a pharmacist, have developed his own proprietary herbal preparation containing oxymatrine and other plant compounds, called Equilibrant.
International Consensus Criteria[edit | edit source]
Dr. Chia co-authored the 2011 case definition, International Consensus Criteria.[4]
Open Letter to The Lancet[edit | edit source]
Three open letters to the editor of The Lancet urged the editor to commission a fully independent review of the PACE trial, which the journal had published in 2011. In 2016, Dr. Chia, along with 41 colleagues in the ME/CFS field, signed the second letter. In 2018, Dr. Chia was joined with over 100 signatories.
- February 10, 2016, An open letter to The Lancet, again - Virology blog[5]
- June 19, 2018, An Open Letter to The Lancet, Two Years On[6]
Notable studies[edit | edit source]
- 2004, Ribavirin and Interferon-α for the Treatment of Patients with Chronic Fatigue Syndrome Associated with Persistent Coxsackievirus B Infection: A Preliminary Observation[7] (Full Text)
- 2005, The role of enterovirus in chronic fatigue syndrome[8] (Full Text)
- 2008, Chronic fatigue syndrome is associated with chronic enterovirus infection of the stomach[9] (Abstract)
- 2010, Antibody to parvovirus B19 nonstructural protein is associated with chronic arthralgia in patients with chronic fatigue syndrome/myalgic encephalomyelitis[10] - (Full Text)
- 2015, Poster - Dr Chia's ME/CFS post-mortem brain study: Chronic Enterovirus Infection in a Patient With Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS) – Clinical, Virologic and Pathological Analysis[11]
- 2015, Functional Dyspepsia and Chronic Gastritis Associated with Enteroviruses[12] (Full Text)
- 2022, Plasma metabolomics reveals disrupted response and recovery following maximal exercise in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome[13] - (Full text)
Talks and interviews[edit | edit source]
- 2008: International Symposium on Viruses In CFS, Baltimore 2008: The Role of Enterovirus in ME/CFS
- 2008: Dr John Chia, Invest in ME International ME Conference, London 2008: The Role of Enterovirus in Chronic Fatigue Syndrome / Myalgic Encephalomyelitis
- 2008, Dr John Chia, Invest in ME International ME Conference, London 2008 Dr John Chia Interview with Professor Malcolm Hooper
- 2009: Dr John Chia, Invest in ME International ME Conference, London 2009: Diagnosis and Treatment of ME/CFS Associated With Chronic Enterovirus Infection
- 2010: Dr John Chia, Invest in ME International ME Conference, London 2010: Enterovirus Infection in ME/CFS
- 2011: Dr John Chia, Invest in ME International ME Conference, London 2011: Clinical and Research Experience of Enteroviral Involvement in ME/CFS
- 2011: Dr John Chia State of Knowledge Workshop on ME/CFS Research (Day 1) Part 1
- 2011: Dr John Chia State of Knowledge Workshop on ME/CFS Research (Day 1) Part 2
- 2011: Dr John Chia State of Knowledge Workshop on ME/CFS Research (Day 2) Review
- 2011: The Dr John Chia Interview – Phoenix Rising: Introduction
- 2012: MECFS Alert Episode 38, part 1 - Interview with Dr. John Chia, Part 1
- 2013: MECFS Alert Episode 39, part 2 - Interview with Dr. John Chia, Part 2
- 2013: MECFS Alert Episode 40, part 3 - Interview with Dr. John Chia, Part 3
- 2013: MECFS Alert Episode 41, part 4 - Interview with Dr. John Chia, Part 4
- 2015: Dr John Chia, Invest in ME International ME Conference, London 2015: Enteroviruses and ME/CFS: An Update on Pathogenesis
- 2016: 12th International IACFS/ME Biennial Clinical and Research Conference: Acute and Chronic Enteroviral Infection
- 2021: Interview with Amy Proal of the PolyBio Research Foundation: Chronic Enterovirus Infections
Media coverage[edit | edit source]
- 2007, Stomach Virus Could Trigger CFS. Enterovirus Found in Many Chronic Fatigue Syndrome Sufferers
- 2007, Study: Common Stomach Virus Tied to Chronic Fatigue
- 2009, Dr. Chia On Oxymatrine, Autoimmunity, ME/CFS and Fibromyalgia
- 2011, An Interview With Dr. John Chia M.D. Enteroviruses and Chronic Fatigue Syndrome Part II: Persistence, Treatment and the Future
- 2011, An Interview With Dr. John Chia, M.D. Part I
- 2011, Dr Chia's report on the use of interferon to treat ME/CFS
- 2011, Oxymatrine
- February 2013, Hanging Fire – Dr. John Chia
Publications[edit | edit source]
- 2003, Correspondence in Clinical Infectious Diseases - "Diverse Etiologies for Chronic Fatigue Syndrome"[14]
Online presence[edit | edit source]
See also[edit | edit source]
- Enterovirus
- Equilibrant
- List of enterovirus infection studies
- Non-cytolytic enterovirus
- Viral testing in ME/CFS
Learn more[edit | edit source]
References[edit | edit source]
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/?term=chia+jk%5Bauthor%5D
- ↑ EVMED Research
- ↑ Ribavirin and Interferon-a for the Treatment of Patients with Chronic Fatigue Syndrome Associated with Persistent Coxsackievirus B Infection: A Preliminary Observation
- ↑ Carruthers, Bruce M.; van de Sande, Marjorie I.; De Meirleir, Kenny L.; Klimas, Nancy G.; Broderick, Gordon; Mitchell, Terry; Staines, Donald; Powles, A.C. Peter; Speight, Nigel; Vallings, Rosamund; Bateman, Lucinda; Baumgarten-Austrheim, Barbara; Bell, David; Carlo-Stella, Nicoletta; Chia, John; Darragh, Austin; Jo, Daehyun; Lewis, Donald; Light, Alan; Marshall-Gradisnik, Sonya; Mena, Ismael; Mikovits, Judy; Miwa, Kunihisa; Murovska, Modra; Pall, Martin; Stevens, Staci (August 22, 2011). "Myalgic encephalomyelitis: International Consensus Criteria". Journal of Internal Medicine. 270 (4): 327–338. doi:10.1111/j.1365-2796.2011.02428.x. ISSN 0954-6820. PMC 3427890. PMID 21777306.
- ↑ Tuller, David (February 10, 2016). "An open letter to The Lancet, again". Virology blog.
- ↑ Tuller, David (June 19, 2018). "Trial By Error: An Open Letter to The Lancet, Two Years On". Virology blog.
- ↑ Chia, John K; Chia, Andrew (2004). "Ribavirin and Interferon-α for the Treatment of Patients with Chronic Fatigue Syndrome Associated with Persistent Coxsackievirus B Infection: A Preliminary Observation" (PDF). The Journal of Applied Research. 4 (2): 286–292.
- ↑ Chia, JKS (2005). "The role of enterovirus in chronic fatigue syndrome". J Clin Pathol. 58 (11): 1126–32. doi:10.1136/jcp.2004.020255. PMID 16254097.
- ↑ Chia, John; Chia, Andrew (2008). "Chronic fatigue syndrome is associated with chronic enterovirus infection of the stomach". Journal of Clinical Pathology. 61 (1): 43–48.
- ↑ Kerr, J.R.; Gough, J.; Richards, S.C.M.; Main, J.; Enlander, D.; McCreary, M.; Komaroff, A.L.; Chia, J.K. (April 1, 2010). "Antibody to parvovirus B19 nonstructural protein is associated with chronic arthralgia in patients with chronic fatigue syndrome/myalgic encephalomyelitis". Journal of General Virology. 91 (4): 893–897. doi:10.1099/vir.0.017590-0. ISSN 0022-1317.
- ↑ "Dr Chia's ME/CFS post-mortem brain study: Chronic Enterovirus Infection in a Patient With Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS) – Clinical, Virologic and Pathological Analysis. John Chia, David Wang, Andrew Chia, Rabiha El-Habbal, 2015. Presented at the 19th International Picornavirus Meeting, 2016".
- ↑ Chia, John K.; Chia, Andrew Y.; Wang, David; El-Habbal, Rabiha (2015), "Functional Dyspepsia and Chronic Gastritis Associated with Enteroviruses", Open Journal of Gastroenterology, 5 (4): 21-27., doi:10.4236/ojgas.2015.54005
- ↑ Germain, Arnaud; Giloteaux, Ludovic; Moore, Geoffrey E.; Levine, Susan M.; Chia, John K.; Keller, Betsy A.; Stevens, Jared; Franconi, Carl J.; Mao, Xiangling; Shungu, Dikoma C.; Grimson, Andrew (March 31, 2022). "Plasma metabolomics reveals disrupted response and recovery following maximal exercise in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". JCI Insight. doi:10.1172/jci.insight.157621. ISSN 0021-9738.
- ↑ Chia, John K.S.; Chia, Andrew (2003), "Diverse Etiologies for Chronic Fatigue Syndrome", Clinical Infectious Diseases, 36 (5): 671-672, doi:10.1086/367666