- This page was created by volunteers like you!
- Help us make it even better. To learn more about contributing to MEpedia, click here.
- Join the movement
- Visit #MEAction to find support or take action. Donate today to help us improve and expand this project.
- Congratulations!
- MEpedia has got over 30 million views as of August 2022!
Myalgic encephalomyelitis
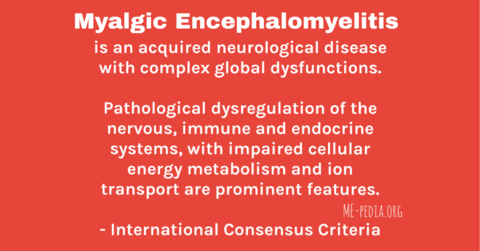
Myalgic encephalomyelitis (ME) is a chronic, inflammatory, physical and neurological and immune-mediated disease that presents with symptoms involving multiple bodily systems. It is frequently triggered by a viral infection or a flu-like illness.[1][2] ME presents with symptoms in the central nervous system (CNS), autonomic nervous system (ANS), immune system, cardiovascular system, endocrine system, digestive system, and musculoskeletal system.[1][3]
Myalgic encephalomyelitis was first classified as a neurological disease by the World Health Organization (WHO) in 1969, with the publication of the World Health Organization's ICD-8 manual.[4]
ME has occurred in both epidemic and sporadic forms.
According to the CDC the hallmark symptom of myalglc encephalomyelitis is post-exertional malaise (PEM), which is the worsening of ME/CFS symptoms after minimal physical, mental, or emotional effort.[5][6][7][8][3] Other key symptoms include muscle weakness and easy muscle fatigability, sleep disturbance, plus either orthostatic intolerance or cognitive dysfunction. Orthostic intolerance is autonomic nervous system dysfunction causing the worsening of symptoms when standing or sitting upright, and may include feeling faint, dizziness, feeling weak, blurred vision, postural orthostatic tachycardia (POTS), reduced heart rate variability at night, and both cold and heat intolerance. Other ME/CFS common symptoms include muscle pain, nerve pain, neck and spine stiffness, and sensory symptoms including sensitivity to light, sound, touch, skin tingling or numbness and hyperaesthesia (skin sensitivity and pain, and allodynia). There is a progressive form of ME, but it is rarer than the relapsing-remitting type.[9]
Among adults, ME is more common in women than men.[2] New onset has been observed in children[10] and in adults usually between the ages of 40-60.[11] Bakken et. al notes two age peaks for CFS/ME; age group 10 to 19 years and a second peak in the age group 30 to 39 years.[12]
There are no approved pharmacological treatments for ME anywhere in the world except in Argentina, which has approved the immunomodulator Ampligen (rintatolimod) for severe ME/CFS as of August 23, 2016.[13]


History[edit | edit source]
Myalgic encephalomyelitis was first classified as a neurological disease by the World Health Organization in 1969, with the publication of the ICD-8 manual.[4]

The World Health Organization's ICD-8 manual did not include any alternative names for myalgic encephalomyelitis although postinfectious encephalomyelitis and all other encephalomyelitis diseases were classified under the same code; fatigue-related alternative names were not added in any later revisions.[4][14] The alternative name chronic fatigue syndrome (CFS) was not in use at this time; it was proposed in 1987 by the Centers for Disease Control, which adopted new diagnostic criteria the following year.[15]:29
In the ICD-9, which was published in 1989, the entry for myalglc encephalomyelitis is uses code 323.9:[16]
ME has occurred in both epidemic and sporadic form since at least the 1930s, although it has likely been occurring much longer but was not formally named. The first recorded outbreak of epidemic myalgic encephalomyelitis was in 1934 in Los Angeles and was thought to be an outbreak of atypical polio. After the outbreak in Akureyri, Iceland in 1946, the disease came to be called Akureyri Disease or Icelandic disease through much of the 1940s and 1950s. It was named ME after London's Royal Free Hospital outbreak in 1955. Other names included benign myalgic encephalomyelitis and epidemic neuromyasthenia.
After the Incline Village outbreak in Nevada in 1984, the disease came to be called and redefined as chronic fatigue syndrome (CFS). The most recent myalgic encephalomyelitis outbreak was caused by the 2019-2022 Coronavirus pandemic outbreak.
Disease name[edit | edit source]

- -myel: relating to the spinal cord.[17]
- -itis: Inflammation.[17]
The name myalgic encephalomyelitis was first used in 1956 in an article in the Lancet medical journal to describ findings from the 1955 Royal Free Hospital outbreak in London, UK.[18][17][19] The term myalgic encephalomyelitis is a portmanteau of several of the key signs and symptoms of the disease: myalgic (muscle pain), encephalo (brain), myel (spinal cord), itis (inflammation).[17][20] The central nervous system (brain and spinal cord) are inflamed.[17]
Benign myalgic encephalomyelitis[edit | edit source]
Benign myalgic encephalomyelitis was the term used by the World Health Organization from 1969,[4] with the prefix "benign" used to denote that M.E. was not fatal, the prefix benign was later dropped since M.E. can cause death, for example the deaths of Merryn Crofts and Sophia Mirza.[17][21][22] Merryn Crofts had very severe ME, was bedbound and unable to eat. Merryn weighed under six stone (84 lbs) at her death, and was just 21 years-old. Merryn's death certificate was the second in the UK to attribute a death to ME.[21]
Disease of a thousand names[edit | edit source]
Myalgic Encephalomyelitis has been referred to as the "disease of a thousand names".[23] Other names used or proposed in the history of the myalgic encephalomyelitis include atypical polio, Icelandic disease, benign ME, epidemic neuromyasthenia, chronic fatigue syndrome, Chronic Fatigue Immune Dysfunction Syndrome (CFIDS), and systemic exertion intolerance disease (SEID).[23][15] This has lead to much confusion as a variety of names have been used at different times to describe discrete outbreaks as well as a larger and potentially more heterogenous population of sporadic cases, defined by a wide variety of diagnostic criteria. Some names have emphasized particular symptoms or pathology, including chronic fatigue syndrome and myalgic encephalomyelitis.[17]
A survey by The MEAction Network in 2016 found that the majority of patients prefer the name ME to other names including chronic fatigue syndrome.[24]
Myalgic encephalomyelitis (ME) was the original name for chronic fatigue syndrome (CFS); the names are sometimes used interchangeably or with the acronym ME/CFS.[20]
Onset[edit | edit source]
According to Dr Byron Hyde, after an incubation period of 4 to 7 days, the prodromal phase generally involve a flu-like illness with low-grade fever.[25] In the majority but not all cases, an infection or infectious process is evident.[25] Two to seven days later, a chronic phase commences, characterized by a measurable diffuse change in the function of the CNS. It is this second phase, persistent phase that most characterizes ME.[26][25]
Signs and symptoms[edit | edit source]
Myalgic encephalomyelitis is a neurological disease that affects multiple bodily systems, causing a widespread combination of symptoms.[27] Symptoms can range from mild to very severe and can include:
- ataxia (coordination difficulties)
- cognitive dysfunction
- fatigability
- gastrointestinal symptoms
- headache
- low-grade fever, temperature instability
- muscle weakness and fatiguability
- myalgia (muscle pain)
- neck and back or spinal cord stiffness
- neuralgia (nerve pain)
- othostatic intolerance
- post-exertional malaise
- sensitivity to heat or cold
- sensitivity to light, sound and/or touch
- sleep dysfunction[27]
Symptom presentation and severity can vary considerably day to day and even hour to hour.[3][28] Overexertion can exacerbate all symptoms, and post-exertional malaise is often delayed by 24 hours or more.[3] The US National Institutes of Health (NIH) notes that sensitivity to noise, light and chemicals may force patients to withdraw from society.[29]
Post-exertional malaise[edit | edit source]
A core symptom, post-exertional malaise (PEM), is intolerance to previously trivial mental or physical effort such as attending a child's school event, running an errand or grocery shopping, taking a shower or brushing teeth; this causes a worsening of symptoms, and deterioration of health from persistent or repeated exertion.[1][3]

Some studies show that patients who have been ill for longer are more likely to uave severe ME/CFS. ME/CFS oftens becomes more severe when patients try to push through their symptoms and continue to repeatedly exceed their personal physical or cognitive limits, for instance by attempting to keep working, which typically entails anaerobic activity.[30][31]
Clinical findings[edit | edit source]

Although there is no definitive biomarker, several signs and findings have been frequently observed in clinical settings:
- high antibody titers to specific infections (including EBV,[32] HHV-6,[33][34] and Coxsackie B[35][36] among others)
- Hormone imbalance[37]
- immunological abnormalities[27][38][39]
- low natural killer cell function[38]
- low red blood cell magnesium[40]
- postural orthostatic tachychardia (POTS)[1][41]
- physical and mental exertion, sensory input cause relapse (PEM)[1][42][3]
Diagnosis[edit | edit source]

There are several proposed criteria for diagnosing ME including the International Consensus Criteria (ICC) and the Canadian Consensus Criteria (CCC). The original criteria developed by Melvin Ramsay, the Ramsay definition, is not used for diagnosing ME today.
Generally accepted criteria for diagnosing ME/CFS and ME[edit | edit source]
- Canadian Consensus Criteria (CCC)[7] A diagnosis of moderate and severe forms of ME/CFS are accurately made using this criterion. Adults can be diagnosed at 6 months while pediatric cases are diagnosed at three months.
- International Consensus Criteria (ICC)[27][1] This criteria will accurately diagnose myalgic encephalomyelitis (ME). There is no requirement that the individual have symptoms for a specified period of time for diagnosis, as opposed to CCC, Fukuda, and SEID, which all require 6 months in adults.
- Systemic Exertion Intolerance Disease (SEID)[15]
ME/CFS (SEID) is accurately diagnosed when the core symptoms are met. The Institute of Medicine report is a whole is a comprehensive review of the medical literature available at time of publication (2015). Adults can be diagnosed at 6 months while pediatric cases are diagnosed at three months.
Other diagnostic criteria[edit | edit source]
Several, overly broad criteria have been proposed and are in use. These criteria likely capture some patients with the disease characterized in the medical literature on epidemic ME, exclude others, and also include patients with a wide range of other undiagnosed conditions including cancer, depression, and a range of autoimmune diseases. The United Kingdom's Oxford criteria for chronic fatigue syndrome is the broadest and likely least discerning definition and has been retired due to the risk of many different fatiguing illnesses being misdiagnosed as chronic fatigue syndrome.[43] The US Centers for Disease Control's (CDC) Fukuda criteria, in use since 1994, is also overly broad. The Institute of Medicine report developed the criteria of Systemic Exertion Intolerance Disease (SEID) and although it can diagnose ME patients with the minimum core symptoms,[44][45] it does not describe the array of symptoms those suffering with ME experience. Symptoms such as neurological, immune/gastrointestinal/genitourinary impairment, and energy metabolism/ion transport impairment; these symptoms are necessary for a diagnosis under the ICC.[27] The CCC requires neurological, autonomic, neuroendocrine, immune system, and myalgia symptoms to meet its ME/CFS diagnostic criteria.[7]
Differential diagnosis[edit | edit source]
The signs and symptoms of myalgic encephalomyelitis can be similar to other medical illnesses, including cancer, multiple sclerosis, lupus, Hashimoto's thyroiditis (hypothyroidism), diabetes mellitus, brucellosis, anemia and others.[46][7] Standard medical tests are needed to help distinguish ME from these other illnesses, and additional testing may also be needed.[45][46][47]
Course and prognosis[edit | edit source]
The prognosis for myalgic encephalomyelitis and chronic fatigue syndrome (ME and CFS) is considered to be poor with only a small minority (a median estimate of 5%) returning to pre-morbid levels of functioning.[48] The majority of patients remains significantly impaired. A substantial improvement however is noted in an estimated 40% of patients[49] and the prognosis in adolescents is considered to be better than in adults.[50][51]
Pathophysiology[edit | edit source]

ME is a multi-system disease. Numerous biological abnormalities have been found in multiple bodily system, however no common, central cause or mechanism has yet been elucidated.
Central nervous system[edit | edit source]

Autonomic nervous system[edit | edit source]
Cardiovascular[edit | edit source]
Gastrointestinal system[edit | edit source]
Immune system[edit | edit source]
Musculoskeletal system[edit | edit source]
Peripheral nervous system[edit | edit source]
Sex differences[edit | edit source]

A Norwegian CFS/ME study shows that the disease affects all ages, with two peak ages of 10-19 years and 30-39 years; it is more common in women than in men.[12] Research by the Open Medicine Foundation cited in its paper, Metabolic features of chronic fatigue syndrome which studied severe CFS, found that the disease is different in men and women but this is not related to testosterone or estrogen. Michael VanElzakker notes there are male and female differences in neuropathic pain. A study of UK and Dutch cohorts found "younger children had a more equal gender balance compared to adolescents and adults."[52]
Risk factors and potential causes[edit | edit source]
Genetic risks[edit | edit source]
Myalgic encephalomyelitis and chronic fatigue syndrome have been reported to run in families, although ME and CFS are not considered inherited illnesses, there is evidence of a genetic predisposition.[53][54][55]
Potential causes[edit | edit source]
Although risk factors for myalgic encephalomyelitis have been identified, no single definitive virus has been found in all cases, which has led to the claim that ME is a common end path of a variety of infectious insults.[56][57] It is still possible ME involves some combination of both environmental and genetic factors. Various theories try to combine the known data into plausible explanations.[58][53] Several theories suggest that ME is an inappropriate immune response to an infection, a theory bolstered by the observation that there is sometimes a family history of autoimmune disease.[59][60] There is also a shift from the Th1 type of helper T cells, which fight infection, to the Th2 type, which are more active in allergy and more likely to attack the body.[61][62]

Viruses[edit | edit source]
Other theories describe ME as an immune response to a chronic infection. The association between ME and the Coxsackie B, Human herpesvirus 6, and HHV-7 viruses[63][64][65] suggests a potential viral contribution in at least some individuals. Some researchers have stated that evidence from epidemic myalgic encephalomyelitis strongly point to an enterovirus, however, in most outbreaks, no virus was successfully isolated.[36][66]
Bacteria[edit | edit source]
Others believe ME may sometimes result from a chronic infection with spirochetal bacteria, such as lyme disease. Another bacterium that has been implicated in ME is chlamydia pneumoniae.[67][68] Protein findings relating to several infections have seen found in the oligoclonal bands ME of patients.[69]
The vagus nerve infection hypothesis (VNIH) accounts for why so many different infectious onsets could be responsible. The vagus nerve runs from the brain stem and throughout the body and has an impact on many body systems.[citation needed]
Transmission via blood[edit | edit source]
Given the uncertainty regarding the cause, ME and CFS patients are barred from [donating blood or organs in the United Kingdom (even after recovery),[70] most of Canada,[71] Australia,[72][73] New Zealand (while symptoms persist), and and for a time also in the United States.[74][75][76]
In the US, the American Association of Blood Banks advises to either accept or defer ME/CFS donors based on "clinical judgment of the donor's health status".[77] Patient charities discourage ME/CFS patients from donating blood,[78]
Treatments[edit | edit source]

There is no cure for ME and no country has approved any pharmacological treatment for the disease except, Argentina which has approved Ampligen for the treatment of severe ME/CFS.[13] However the effectiveness of Ampligen is under dispute.[79] Other medications have been used off-label for ME with varying effectiveness in some patients.[7][27]
Treatments for sleep problems, headaches, pain or other symptoms are utilized by some doctors for some patients although these are treating symptoms and not ME itself.[27]
Success of treating symptoms of ME is not well researched or documented.
An immune system modulator drug called Rituximab has failed in a phase III clinical trial.[80] The antiviral Valganciclovir failed in a controlled nine month study against ME patients positive for Herpes Simplex 6 and Epstein Barr viral infections.[81]
Epidemiology[edit | edit source]
ME has been found world-wide, in at least 75 epidemics documented in published papers from the 1930s to the 1980s.[82] Epidemics often occur in enclosed communities such as schools and hospitals.
As observed in many autoimmune disorders, ME is more common in females than males; the mean sex ratio is approximately 2-3 females for every male.[12] In children the sex ratio is approximately equal.[52]
Co-morbidities[edit | edit source]

Clinicians have observed several predisposing conditions, co-morbidities, overlapping conditions, and increased risks for secondary diseases in patients with ME.[7][3] However, as no large-scale epidemiological studies, genetic studies, or family studies have been done, there is little that can be said definitively about the rate or underlying biological reasons for these potentially related conditions. Overlapping diagnostic criteria and the lack of a biomarker in many of these conditions add to the confusion and diagnostic uncertainty. Moreover, certain conditions such as postural orthostatic tachycardia syndrome (POTS) and neurally mediated hypotension (NMH) and idiopathic intracranial hypertension (IIH/IH) and fibromyalgia (FM/FMS) can occur in or be co-morbid with numerous conditions, including ME.[39][83]
The following are some syndromes and diseases that have been associated with or misdiagnosed as ME:
- fibromyalgia[84]
- Lyme disease and chronic Lyme disease[27]
- idiopathic intracranial hypertension[83]
- postural orthostatic tachychardia syndrome[27][85]
- irritable bowel syndrome[84][7]
- Hashimoto's thyroiditis (hypothyroidism)[46]
- Ehlers-Danlos syndrome[46]
- Sjögren's syndrome[46]
- multiple chemical sensitivity[84][1]
A Swedish study of 234 ME/CFS patients meeting the Canadian Consensus Criteria found that 13.2% had tonsillar herniations severe enough to be considered a Chiari Malformation. 49% had hypermobility and 20% met criteria for hEDS (Ehlers-Danlos syndrome with hypermobility), while 96% had fibromyalgia trigger point pain, with 67% meeting the diagnostic criteria for fibromyalgia.[86]
Notable studies[edit | edit source]
Due to lack of funding by governments around the world there has been little biological research into ME/CFS. There are studies which do reveal neurological involvement, metabolic features, and other abnormalities.
- 2016, Metabolic features of chronic fatigue syndrome
- 2016, CDC Multi-site Clinical Assessment of CFS
- 2019, Evidence of widespread metabolite abnormalities in Myalgic encephalomyelitis/chronic fatigue syndrome: assessment with whole-brain magnetic resonance spectroscopy
- List of abnormal findings in chronic fatigue syndrome and myalgic encephalomyelitis
News and articles[edit | edit source]
- 2015, US NIH Report Calls for UK Definition of ME/CFS to be Scrapped - The Argus Report
- 2014, Brains of People With Chronic Fatigue Syndrome Offer Clues About Disorder
- 2010, Chronic fatigue patients barred from blood donation - Washington Post
- 1987, Fatigue 'Virus' Has Experts More Baffled And Skeptical Than Ever - The New York Times
See also[edit | edit source]
- Chronic fatigue syndrome
- Misdiagnosis of myalgic encephalomyelitis and chronic fatigue syndrome
- ME/CFS
- Pediatric myalgic encephalomyelitis and chronic fatigue syndrome
- Severe and very severe ME
- Systemic Exertion Intolerance Disease
Learn more[edit | edit source]
- What is ME/CFS? - CDC
- Diagnosis - Other conditions for evaluation - CDC
- Evaluation - medical tests needed to rule out other illnesses from ME/CFS - CDC
- M.E. International Consensus Criteria
References[edit | edit source]
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Carruthers, BM; van de Sande, MI; De Meirleir, KL; Klimas, NG; Broderick, G; Mitchell, T; Staines, D; Powles, ACP; Speight, N; Vallings, R; Bateman, L; Bell, DS; Carlo-Stella, N; Chia, J; Darragh, A; Gerken, A; Jo, D; Lewis, DP; Light, AR; Light, KC; Marshall-Gradisnik, S; McLaren-Howard, J; Mena, I; Miwa, K; Murovska, M; Stevens, SR (2012), Myalgic encephalomyelitis: Adult & Paediatric: International Consensus Primer for Medical Practitioners (PDF), ISBN 978-0-9739335-3-6
- ↑ Jump up to: 2.0 2.1 "Possible Causes | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. January 18, 2019. Retrieved April 13, 2019.
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 3.5 3.6 "Symptoms | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. May 18, 2018. Retrieved November 21, 2018.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 World Health Organization (1969). Manual of the International Statistical Classification of Diseases, Injuries, and Causes of Death Based on the Recommendations of the Eighth Revision Conference (PDF). 2 (8th ed.). Geneva: WHO. p. 173.
Encephalomyelitis (chronic),
(myalgic, benign) 323 - ↑ "Information for Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. December 27, 2021. Retrieved March 28, 2022.
- ↑ Friedman, Kenneth J.; Murovska, Modra; Pheby, Derek F.H.; Zalewski, Paweł (March 2021). "Our Evolving Understanding of ME/CFS". Medicina. 57 (3): 200. doi:10.3390/medicina57030200. ISSN 1648-9144. PMID 33652622.
- ↑ Jump up to: 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Carruthers, Bruce M.; Jain, Anil Kumar; De Meirleir, Kenny L.; Peterson, Daniel L.; Klimas, Nancy G.; Lerner, A. Martin; Bested, Alison C.; Flor-Henry, Pierre; Joshi, Pradip; Powles, AC Peter; Sherkey, Jeffrey A.; van de Sande, Marjorie I. (2003), "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols" (PDF), Journal of Chronic Fatigue Syndrome, 11 (2): 7–115, doi:10.1300/J092v11n01_02
- ↑ Speight, Nigel (2013). "Myalgic encephalomyelitis/chronic fatigue syndrome: Review of history, clinical features, and controversies". Saudi J Med Med Sci. 1 (1): 11–13. doi:10.4103/1658-631x.112905.
- ↑ Howes, S; Goudsmit, EM (July 7, 2015). "Progressive Myalgic Encephalomyelitis (ME) or A New Disease? A Case Report" (PDF). Physical Medicine and Rehabilitation - International. 2 (6): 1052.
- ↑ "ME/CFS in Children | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. January 18, 2019. Retrieved April 13, 2019.
- ↑ "What is ME/CFS? | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. January 18, 2019. Retrieved April 13, 2019.
- ↑ Jump up to: 12.0 12.1 12.2 Bakken, Inger Johanne; Tveito, Kari; Gunnes, Nina; Ghaderi, Sara; Stoltenberg, Camilla; Trogstad, Lill; Håberg, Siri Eldevik; Magnus, Per (October 1, 2014). "Two age peaks in the incidence of chronic fatigue syndrome/myalgic encephalomyelitis: a population-based registry study from Norway 2008-2012". BMC Medicine. 12 (1): 167. doi:10.1186/s12916-014-0167-5. ISSN 1741-7015. PMC 4189623. PMID 25274261.
- ↑ Jump up to: 13.0 13.1 Hemispherx Biopharma, Inc (August 23, 2016). "Hemispherx Biopharma Announces Major Breakthrough: Approval for Commercial Sale of Rintatolimod (U.S. Tradename: Ampligen®) to Treat Severe Cases of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) in the Argentine Republic". GlobeNewswire News Room. Retrieved August 12, 2018.
- ↑ World Health Organization (2016). "G93 Other diseases of the nervous system - ICD-10 Version:2016". World Health Organization. Retrieved April 13, 2019.
- ↑ Jump up to: 15.0 15.1 15.2 Institute of Medicine (2015). Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness. Washington, DC: The National Academies Press. doi:10.17226/19012.
- ↑ World Health Organization & International Conference for the Ninth Revision of the International Classification of Diseases (1978). Manual of the international statistical classification of diseases, injuries, and causes of death : based on the recommendations of the ninth revision conference, 1975, and adopted by the Twenty-ninth World Health Assembly, 1975 revision: alphabetic index (PDF). 2 (9th ed.). Geneva: World Health Organization. p. 182. ISBN 9241540044.
- ↑ Jump up to: 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 17.8 Hooper, Malcolm. "The Terminology of ME & CFS".
- ↑ "A new clinical entity?" (PDF). Lancet. 1: 789–790. 1956.
- ↑ Ramsay, A. Melvin (October 30, 1965). "Hysteria and "Royal Free Disease."". British Medical Journal. 2 (5469): 1062. ISSN 0007-1447. PMC 1847119.
- ↑ Jump up to: 20.0 20.1 Smith, David G (1989). Understanding M.E.: The Phenomenon of Myalgic Encephalomyelitis and Acute Onset Post Viral Fatigue Syndrome. p. 20.
- ↑ Jump up to: 21.0 21.1 Taylor, Jim (July 27, 2018). "'Vindication' for woman who wanted ME on death certificate". BBC Radio 5 Live.
- ↑ World Health Organization. "8E49 Postviral fatigue syndrome | ICD-11 - Mortality and Morbidity Statistics". World Health Organization. Retrieved March 19, 2022.
8E49 Postviral fatigue syndrome
Other disorders of the nervous system
Inclusions
chronic fatigue syndrome
myalgic encephalomyelitis
Exclusions
Fatigue (MG22) - ↑ Jump up to: 23.0 23.1 Bell, David S. (1991). Chronic Fatigue/Immune Dysfunction Syndrome. CFIDS: The disease of a thousand names. Lyndonville, NY: Pollard Publications. Archived from the original on February 16, 2010.
- ↑ "#MEAction RFI Poll Report (Part 1 of 3) - #MEAction". #MEAction. August 7, 2016. Retrieved September 8, 2018.
- ↑ Jump up to: 25.0 25.1 25.2 Evans, Meredyth; Jason, Leonard (2018). "Onset patterns of chronic fatigue syndrome and myalgic encephalomyelitis" (PDF). Research on Chronic diseases. 2 (1): 2–3.
- ↑ Hyde, Byron (2016), The Nightingale Research Foundation Definition of Myalgic Encephalomyelitis (M.E.), IACFS/ME
- ↑ Jump up to: 27.0 27.1 27.2 27.3 27.4 27.5 27.6 27.7 27.8 Carruthers, Bruce M.; van de Sande, Marjorie I.; De Meirleir, Kenny L.; Klimas, Nancy G.; Broderick, Gordon; Mitchell, Terry; Staines, Donald; Powles, A.C. Peter; Speight, Nigel; Vallings, Rosamund; Bateman, Lucinda; Baumgarten-Austrheim, Barbara; Bell, David; Carlo-Stella, Nicoletta; Chia, John; Darragh, Austin; Jo, Daehyun; Lewis, Donald; Light, Alan; Marshall-Gradisnik, Sonya; Mena, Ismael; Mikovits, Judy; Miwa, Kunihisa; Murovska, Modra; Pall, Martin; Stevens, Staci (August 22, 2011). "Myalgic encephalomyelitis: International Consensus Criteria". Journal of Internal Medicine. 270 (4): 327–338. doi:10.1111/j.1365q-2796.2011.02428.x. ISSN 0954-6820. PMC 3427890. PMID 21777306.
- ↑ International Association for Chronic Fatigue Syndrome / Myalgic Encephalomyelitis; Friedberg, Fred; Bateman, Lucinda; Bested, Alison C; Davenport, Todd; Friedman, Kenneth J; Gurwitt, Alan R; Jason, Leonard A; Lapp, Charles W; Stevens, Staci R; Underhill, Rosemary A; Vallings, Rosamund (2014), Chronic Fatigue Syndrome Myalgic Encephalomyelitis Primer for Clinical Practitioners (PDF), Chicago, USA: International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis,
The illness can vary from mild to severe, with symptoms that may fluctuate significantly from hour to hour and day to day.
- ↑ "ME/CFS - Pathways to Prevention - Advancing the Research on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". National Institutes of Health. December 8, 2016. Retrieved March 28, 2022.
Effects of the illness can range from moderate to debilitating, and can substantially impact everyday functioning. Routine daily activities such as cooking meals, brushing teeth, and caring for children become difficult. Additionally, sensitivity to environmental factors (e.g., noise, light, chemicals) may force many individuals with ME/CFS into seclusion or withdrawal from society.
- ↑ Jump up to: 30.0 30.1 Vink, Mark (September 10, 2015). "The Aerobic Energy Production and the Lactic Acid Excretion are both Impeded in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Journal of Neurology and Neurobiology (ISSN 2379-7150). 1. doi:10.16966/2379-7150.112.
- ↑ Vink, Mark; Vink-Niese, Alexandra (September 20, 2019). "Work Rehabilitation and Medical Retirement for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients. A Review and Appraisal of Diagnostic Strategies". Diagnostics. 9 (4): 124. doi:10.3390/diagnostics9040124. ISSN 2075-4418.
People with ME/CFS often feel under pressure to continue working when they first become ill or when their symptoms worsen. Unfortunately, trying to push through this illness is counterproductive, potentially causing longer sickness absences and slower recovery.
- ↑ Schmaling, K.B.; Jones, J.F. (January 1996). "MMPI profiles of patients with chronic fatigue syndrome". Journal of Psychosomatic Research. 40 (1): 67–74. ISSN 0022-3999. PMID 8730646.
- ↑ Cuende JI, Civeira P, Diez N, Prieto J (1997). "[High prevalence without reactivation of herpes virus 6 in subjects with chronic fatigue syndrome]". An Med Interna. 14 (9): 441–4. PMID 9453750.
- ↑ Komaroff, AL (2006). "Is human herpesvirus-6 a trigger for chronic fatigue syndrome?". J Clin Virol. 37 (Suppl 1): S39-46. doi:10.1016/S1386-6532(06)70010-5. PMID 17276367.
- ↑ Landay, AL (September 1991). "Chronic fatigue syndrome: clinical condition associated with immune activation". Lancet.
- ↑ Jump up to: 36.0 36.1 Chia, John (November 2005). "The role of enterovirus in chronic fatigue syndrome". Journal of Clinical Pathology.
- ↑ Ruiz-Núñez, Begoña; Tarasse, Rabab; Vogelaar, Emar F.; Janneke Dijck-Brouwer, D.A.; Muskiet, Frits A. J. (2018). "Higher Prevalence of "Low T3 Syndrome" in Patients With Chronic Fatigue Syndrome: A Case–Control Study". Frontiers in Endocrinology. 9: 97. doi:10.3389/fendo.2018.00097. PMID 29615976.
- ↑ Jump up to: 38.0 38.1 Brenu, Ekua Weba; Huth, Teilah K.; Hardcastle, Sharni L.; Fuller, Kirsty; Kaur, Manprit; Johnston, Samantha; Ramos, Sandra B.; Staines, Don R.; Marshall-Gradisnik, Sonya M. (April 2014). "Role of adaptive and innate immune cells in chronic fatigue syndrome/myalgic encephalomyelitis". International Immunology. 26 (4): 233–242. doi:10.1093/intimm/dxt068. ISSN 1460-2377. PMID 24343819.
- ↑ Jump up to: 39.0 39.1 "Etiology and Pathophysiology | Presentation and Clinical Course | Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. November 8, 2018. Retrieved February 17, 2019.
- ↑ Cox, I.M.; Campbell, M.J.; Dowson, D. (March 30, 1991). "Red blood cell magnesium and chronic fatigue syndrome". Lancet (London, England). 337 (8744): 757–760. ISSN 0140-6736. PMID 1672392.
- ↑ "Overlapping Conditions – American ME and CFS Society". ammes.org. Retrieved August 12, 2018.
- ↑ Arroll, Megan A.; Attree, Elizabeth A.; O'Leary, John M.; Dancey, Christine P. (April 3, 2014). "The delayed fatigue effect in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)". Fatigue: Biomedicine, Health & Behavior. 2 (2): 57–63. doi:10.1080/21641846.2014.892755. ISSN 2164-1846.
- ↑ Haney, Elizabeth; Smith, M.E. Beth; McDonagh, Marian; Pappas, Miranda; Daeges, Monica; Wasson, Ngoc; Nelson, Heidi D. (June 16, 2015). "Diagnostic Methods for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Systematic Review for a National Institutes of Health Pathways to Prevention Workshop". Annals of Internal Medicine. 162 (12): 834. doi:10.7326/m15-0443. ISSN 0003-4819.
- ↑ "Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness - Diagnostic Algorithm". nationalacademies.org. 2015.
- ↑ Jump up to: 45.0 45.1 "Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome - Redefining an Illness: Clinicians' Guide" (PDF). National Academies. 2015.
- ↑ Jump up to: 46.0 46.1 46.2 46.3 46.4 "Other Conditions for Evaluation | Information for Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. July 12, 2018. Retrieved March 28, 2022.
- ↑ "Evaluation | Information for Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. April 28, 2021. Retrieved April 1, 2022.
- ↑ Cairns, R.; Hotopf, M. (January 2005). "A systematic review describing the prognosis of chronic fatigue syndrome". Occupational Medicine (Oxford, England). 55 (1): 20–31. doi:10.1093/occmed/kqi013. ISSN 0962-7480. PMID 15699087.
- ↑ Joyce, J.; Hotopf, M.; Wessely, S. (March 1997). "The prognosis of chronic fatigue and chronic fatigue syndrome: a systematic review". QJM: monthly journal of the Association of Physicians. 90 (3): 223–233. ISSN 1460-2725. PMID 9093600.
- ↑ "Prognosis | Presentation and Clinical Course | Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. July 10, 2018. Retrieved October 28, 2018.
- ↑ Rowe, Peter C.; Underhill, Rosemary A.; Friedman, Kenneth J.; Gurwitt, Alan; Medow, Marvin S.; Schwartz, Malcolm S.; Speight, Nigel; Stewart, Julian M.; Vallings, Rosamund (2017). "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Diagnosis and Management in Young People: A Primer". Frontiers in Pediatrics. 5. doi:10.3389/fped.2017.00121. ISSN 2296-2360.
- ↑ Jump up to: 52.0 52.1 Collin, Simon M.; Nuevo, Roberto; van de Putte, Elise M.; Nijhof, Sanne L.; Crawley, Esther (October 28, 2015). "Chronic fatigue syndrome (CFS) or myalgic encephalomyelitis (ME) is different in children compared to in adults: a study of UK and Dutch clinical cohorts". BMJ open. 5 (10): e008830. doi:10.1136/bmjopen-2015-008830. ISSN 2044-6055. PMID 26510728.
- ↑ Jump up to: 53.0 53.1 Schlauch, Karen A.; Khaiboullina, Svetlana F.; De Meirleir, Kenny L.; Rawat, Shanti; Petereit, J; Rizvanov, Albert A; Blatt, Nataliya; Mijatovic, Tatjana; Kulick, D; Palotás, András; Lombardi, Vincent C. (2016). "Genome-wide association analysis identifies genetic variations in subjects with myalgic encephalomyelitis/chronic fatigue syndrome". Translational Psychiatry. 6 (2): e730. doi:10.1038/tp.2015.208.
- ↑ Dibble, Joshua J; McGrath, Simon J; Ponting, Chris P (August 3, 2020). "Genetic risk factors of ME/CFS: a critical review". Human Molecular Genetics. 29 (R1): R117–R124. doi:10.1093/hmg/ddaa169. ISSN 0964-6906. PMC 7530519. PMID 32744306.
- ↑ Hajdarevic, Riad; Lande, Asgeir; Mehlsen, Jesper; Rydland, Anne; Sosa, Daisy D.; Strand, Elin B.; Mella, Olav; Pociot, Flemming; Fluge, Øystein; Lie, Benedicte A.; Viken, Marte K. (May 1, 2022). "Genetic association study in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) identifies several potential risk loci". Brain, Behavior, and Immunity. 102: 362–369. doi:10.1016/j.bbi.2022.03.010. ISSN 0889-1591.
- ↑ Rasa, Santa; Nora-Krukle, Zaiga; Henning, Nina; Eliassen, Eva; Shikova, Evelina; Harrer, Thomas; Scheibenbogen, Carmen; Murovska, Modra; Prusty, Bhupesh K.; European Network on ME/CFS (EUROMENE) (October 1, 2018). "Chronic viral infections in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)". Journal of Translational Medicine. 16 (1). doi:10.1186/s12967-018-1644-y. ISSN 1479-5876. PMID 30285773.
- ↑ Magnus, Per; Gunnes, Nina; Tveito, Kari; Bakken, Inger Johanne; Ghaderi, Sara; Stoltenberg, Camilla; Hornig, Mady; Lipkin, W. Ian; Trogstad, Lill (November 17, 2015). "Chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) is associated with pandemic influenza infection, but not with an adjuvanted pandemic influenza vaccine". Vaccine. 33 (46): 6173–6177. doi:10.1016/j.vaccine.2015.10.018. ISSN 1873-2518. PMID 26475444.
- ↑ Underhill, R.A. (2015). "Myalgic encephalomyelitis, chronic fatigue syndrome: An infectious disease". Medical Hypotheses. 85 (6): 765–773. doi:10.1016/j.mehy.2015.10.011. ISSN 1532-2777. PMID 26604026.
- ↑ Sotzny, Franziska; Blanco, Julià; Capelli, Enrica; Castro-Marrero, Jesús; Steiner, Sophie; Murovska, Modra; Scheibenbogen, Carmen (2018). "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome – Evidence for an autoimmune disease". Autoimmunity Reviews. 17 (6): 601-609. doi:10.1016/j.autrev.2018.01.009.
- ↑ "Klimas ME CFS Genes Study". facebook.com. November 23, 2015. Retrieved September 8, 2018.
- ↑ "Cytokine expression provides clues to the pathophysiology of Gulf War illness and myalgic encephalomyelitis". Cytokine. 72 (1): 1–8. March 1, 2015. doi:10.1016/j.cyto.2014.11.019. ISSN 1043-4666.
- ↑ Hardcastle, S.L.; Brenu, E.W.; Staines, D.R.; Marshall-Gradisnik, S. (2014). "Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and the Potential Role of T Cells" (PDF). Biological Markers and Guided Therapy. 1 (1=): 25. doi:10.12988/bmgt.2014.3122.
- ↑ Bell, E.J.; McCartney, R.A.; Riding, M.H. (1988). "Coxsackie B viruses and myalgic encephalomyelitis". Journal of the Royal Society of Medicine. 81 (6): 329–331. doi:10.1177/014107688808100609. ISSN 0141-0768. PMID 2841461.
- ↑ "Ramsay Research Team 5 – The Potential Role of HHV-6 in ME/CFS - Solve ME/CFS Initiative". Solve ME/CFS Initiative. VOLKMEDIA. December 16, 2016. Retrieved September 8, 2018.
- ↑ Chapenko, Svetlana; Krumina, Angelika; Logina, Inara; Rasa, Santa; Chistjakovs, Maksims; Sultanova, Alina; Viksna, Ludmila; Murovska, Modra (2012). "Association of active human herpesvirus-6, -7 and parvovirus b19 infection with clinical outcomes in patients with myalgic encephalomyelitis/chronic fatigue syndrome". Advances in Virology: 205085. doi:10.1155/2012/205085. ISSN 1687-8647. PMID 22927850.
- ↑ O'Neal, Adam J.; Hanson, Maureen R. (2021). "The Enterovirus Theory of Disease Etiology in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Critical Review". Frontiers in Medicine. 8: 688486. doi:10.3389/fmed.2021.688486/abstract. ISSN 2296-858X.
- ↑ Tovey, JE (September 5, 2018). "Chlamydia pneumoniae infection a treatable cause of Chronic Fatigue Syndrome". The BMJ.
- ↑ "New ME/CFS Study at Stanford: Dr. Montoya to test for scores of Infections - Prohealth". Prohealth. June 4, 2010. Retrieved September 8, 2018.
- ↑ Nicolson, Garth L.; Haier, Jörg (2009). "Role of Chronic Bacterial and Viral Infections in Neurodegenerative, Neurobehavioral, Psychiatric, Autoimmune and Fatiguing Illnesses: Part 1". British Journal of Medical Practitioners. 2 (4): 20–28.
- ↑ "Knowledgebase". My Donor Record - Health, Eligibility & Travel. Retrieved October 8, 2021.
- ↑ Wilson, Kumanan; Atkinson, Katherine; Keelan, Jennifer (April 8, 2014). "The Use of Preliminary Scientific Evidence in Public Health: A Case Study of XMRV". PLOS Medicine. 11 (4): e1001623. doi:10.1371/journal.pmed.1001623. ISSN 1549-1676. PMC 3979645. PMID 24714396.
- ↑ "Chronic Fatigue Syndrome". Australian Red Cross. Retrieved November 17, 2023.
- ↑ "Chronic fatigue syndrome – I have/had chronic fatigue syndrome. Can I donate?". Australian Red Cross. Retrieved May 25, 2022.
- ↑ Stein, Rob (December 3, 2010). "Red Cross bars chronic fatigue patients from donating blood". Washington Post. Retrieved May 25, 2022.
- ↑ Stein, Rob (December 3, 2010). "Chronic fatigue patients barred from blood donation". Washington Post. ISSN 0190-8286. Retrieved September 8, 2018.
- ↑ "Detailed eligibility criteria". NZ Blood. Retrieved September 8, 2018.
- ↑ American Association of Blood Banks (October 2012). "Xenotropic Murine Leukemia Virus-Related Virus (XMRV) and other Polytropic Murine Leukemia Viruses (pMLV)" (PDF). p. 3. Retrieved May 25, 2022.
An updated AABB Association Bulletin #12-05 (November 2012) states that individual collectors of blood and cellular therapy products should accept or defer donors with a history of CFS based on their clinical judgment of the donor's health status.
- ↑ "AABB's recommendation on ME/CFS and blood donation". Massachusetts ME/CFS & FM Association. November 25, 2015. Retrieved May 25, 2022.
- ↑ George, John (December 2, 2009). "FDA rejects Hemispherx's chronic fatigue drug Ampligen". bizjournals.com. Retrieved August 12, 2018.
- ↑ Johnson, Cort (November 26, 2017). "Norwegian Rituximab Chronic Fatigue Syndrome (ME/CFS) Trial Fails - Simmaron Research". Simmaron Research. Retrieved September 7, 2018.
- ↑ Montoya, Jose G.; Kogelnik, Andreas M.; Bhangoo, Munveer; Lunn, Mitchell R.; Flamand, Louis; Merrihew, Lindsey E.; Watt, Tessa; Kubo, Jessica T.; Paik, Jane (December 2013). "Randomized clinical trial to evaluate the efficacy and safety of valganciclovir in a subset of patients with chronic fatigue syndrome". Journal of Medical Virology. 85 (12): 2101–2109. doi:10.1002/jmv.23713. ISSN 1096-9071. PMID 23959519.
- ↑ Bassett, Jodi (September 2010). "M.E.: The medical facts". The Hummingbirds' Foundation for M.E. Retrieved September 8, 2018.
- ↑ Jump up to: 83.0 83.1 Dankaerts, Wim; Bruyninckx, Frans; Stalmans, Ingeborg; Vansant, Greet; Rasschaert, Ricky; Hulens, Mieke (December 10, 2018). "The link between idiopathic intracranial hypertension, fibromyalgia, and chronic fatigue syndrome: exploration of a shared pathophysiology". Journal of Pain Research. Retrieved February 17, 2019.
- ↑ Jump up to: 84.0 84.1 84.2 "Comorbid Conditions | Diagnosis | Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. November 8, 2018. Retrieved February 26, 2019.
- ↑ Hoad, A.; Spickett, G.; Elliott, J.; Newton, J. (2008). "Postural orthostatic tachycardia syndrome is an under-recognized condition in chronic fatigue syndrome". QJM: monthly journal of the Association of Physicians. 101 (12): 961–965. doi:10.1093/qjmed/hcn123. ISSN 1460-2393. PMID 18805903.
- ↑ Bragée, Björn; Michos, Anastasios; Drum, Brandon; Fahlgren, Mikael; Szulkin, Robert; Bertilson, Bo C. (2020). "Signs of Intracranial Hypertension, Hypermobility, and Craniocervical Obstructions in Patients With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Frontiers in Neurology. 11. doi:10.3389/fneur.2020.00828. ISSN 1664-2295.